Sat Sharma received the AADSM Clinical Research Award for demonstrating that sleep apnea-specific hypoxic burden is a more accurate predictor of OSA-related risk and treatment efficacy than the traditional AHI.
Summary: Sat Sharma, the medical director of the Centre for Sleep and Chronobiology and chief medical officer of Open Airway Dental Solutions, has been awarded the American Academy of Dental Sleep Medicine Clinical Research Award for his research demonstrating that sleep apnea-specific hypoxic burden is a more reliable indicator of obstructive sleep apnea (OSA)-related cardiovascular risk and treatment efficacy than the traditional apnea-hypopnea index (AHI). Sharma and co-investigators assessed the effectiveness of the O2Vent Optima oral appliance combined with the ExVent accessory in reducing hypoxic burden in OSA patients.
Three Key Takeaways:
- Sat Sharma’s study, honored with the AADSM Clinical Research Award, reveals that sleep apnea-specific hypoxic burden may be a superior predictor of OSA-related cardiovascular risk compared to the commonly used apnea-hypopnea index (AHI).
- The research showed that treatment with the O2Vent Optima oral appliance and the ExVent accessory reduced AHI from 22.5 to 7.9 events per hour and sleep apnea-specific hypoxic burden from 62.3 to 18.7 %min/hr, with a higher therapeutic efficacy when measured by hypoxic burden (94%) compared to AHI (76%).
- The study suggests that relying solely on AHI measurements for assessing therapeutic efficacy may misclassify many patients who respond well to treatment, emphasizing the importance of incorporating hypoxic burden metrics in evaluating OSA treatments.
Sat Sharma, MD, FRCPC, FCCP, FACP, FAASM, medical director of the Centre for Sleep and Chronobiology and chief medical officer of Open Airway Dental Solutions, has been honored with an American Academy of Dental Sleep Medicine Clinical Research Award for his research on the predictive value of sleep apnea-specific hypoxic burden over the apnea-hypopnea index (AHI) in assessing obstructive sleep apnea (OSA)-related risk.
Studies have shown that sleep apnea-specific hypoxic burden is more predictive of OSA-related cardiovascular risk than the commonly used AHI. However, sleep apnea-specific hypoxic burden has not been extensively studied as a measure of therapeutic efficacy in patients treated with oral appliance therapy, according to the abstract by Sharma and co-investigators.
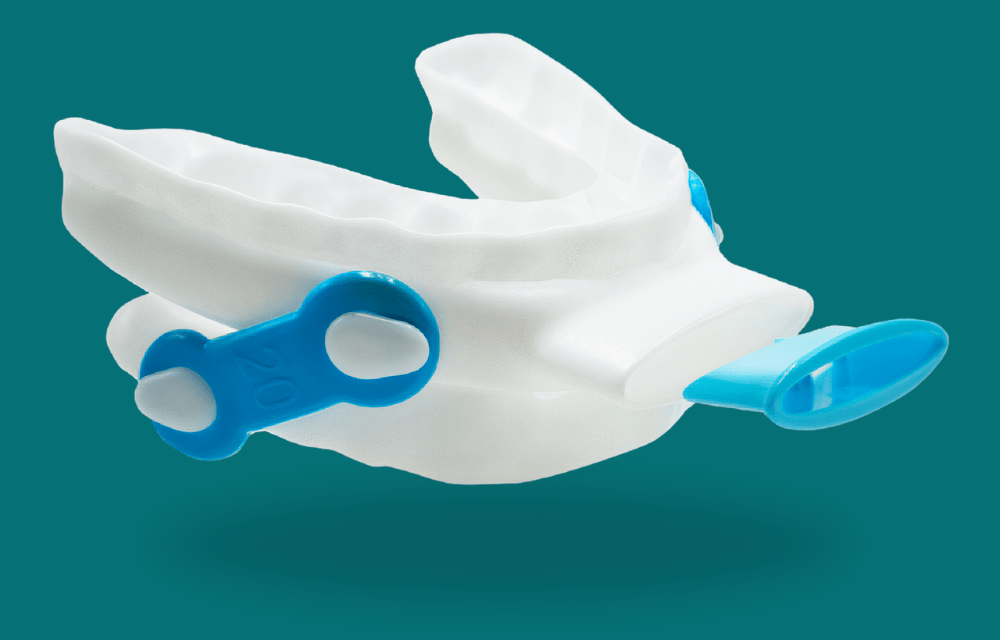
The study evaluates the effectiveness of Open Airway Dental Solutions’ O2Vent Optima oral appliance combined with an oral expiratory positive airway pressure accessory, ExVent (investigational use only—FDA submission completed).

Treatment Approach
The O2Vent Optima is an oral appliance designed to reduce pharyngeal collapsibility through mandibular advancement while incorporating an air channel to circumvent nasopharyngeal obstruction. The ExVent is an optional accessory to the O2Vent Optima that provides oral expiratory positive airway pressure, supporting the upper airway by passive dilation, thereby reducing flow limitation.
This research assesses the combination of the O2Vent Optima and the ExVent accessory in reducing sleep apnea-specific hypoxic burden rather than relying solely on AHI to define therapeutic efficacy.
Materials and Methods
Data were obtained from a clinical study assessing the efficacy of the O2Vent Optima combined with the ExVent accessory in treating OSA. Twenty-four participants with mild to moderate OSA (10 mild, 14 moderate) completed a diagnostic polysomnography (PSG) study to establish baseline AHI and confirm their OSA diagnosis.
Participants used the O2Vent Optima with ExVent at home for over three months, logging their usage hours. Following this period, subjects underwent an in-lab PSG sleep study while using the O2Vent Optima and ExVent.
Results
Treatment with the O2Vent Optima and ExVent reduced AHI from 22.5 ± 6.4/hr to 7.9 ± 2.7/hr (p < 0.001) and sleep apnea-specific hypoxic burden from 62.3 ± 34.1 %min/hr to 18.7 ± 25.4 %min/hr (p < 0.001). The average reduction in AHI was 72%. Using an AHI-based definition of therapeutic efficacy (AHI < 10/hr), 76% of participants achieved efficacy with the O2Vent Optima and ExVent.
However, when using the sleep apnea-specific hypoxic burden-based definition of therapeutic efficacy (sleep apnea-specific hypoxic burden < 53 %min/hr), the therapeutic efficacy increased to 94%.
The findings suggest that relying solely on AHI measurements would misclassify a substantial number of individuals who respond to the therapy, underscoring the importance of sleep apnea-specific hypoxic burden in evaluating OSA-related risk reduction.